A congenital condition occurring during fetal development, Spina Bifida results from the incomplete formation of the spine and spinal cord due to a neural tube defect. This defect causes the spine and spinal cord to be exposed or protrude through an opening in the back, leading to varying degrees of severity, from mild to severe. As a result, individuals may experience physical and cognitive challenges, including weakness or paralysis in the legs, bladder and bowel control issues, learning disabilities, and hydrocephalus, a condition characterized by fluid accumulation in the brain. Early detection and intervention are crucial in managing Spina Bifida and improving quality of life for those affected, enabling individuals and families to navigate this complex condition with support and resources.
Reference: Spina Bifida
Types of Spina Bifida
Spina Bifida encompasses three distinct categories, each characterized by varying degrees of spinal cord and membrane involvement.
Spina Bifida Occulta
This mild form features a small opening in the spine, leaving the spinal cord and nerves intact but potentially covered by a thin membrane. While often asymptomatic, Spina Bifida Occulta may cause minor issues like back pain or skin problems.
Meningocele
In this moderate form, a membrane bulges through the spinal opening, while the spinal cord remains inside. Meningocele can lead to symptoms ranging from mild to moderate, including bladder and bowel control issues, weakness, or paralysis.
Myelomeningocele
The most severe form, Myelomeningocele, involves the protrusion of both the spinal cord and membrane through the spinal opening. This exposure can result in significant physical and cognitive disabilities, necessitating surgical intervention and ongoing management.

Reference: Different Types
Causes and Risk Factors
There is no single cause of Spina Bifida, but there may be a complex exchange of hereditary and natural components that contribute to its improvement. Investigate recommends that people with a family history of the condition are more likely to be influenced, as hereditary changes can affect spinal line arrangement. Furthermore, eager moms who have diabetes, are hefty or have a folic corrosive insufficiency amid pregnancy increase the chance of their child creating Spina Bifida. Certain solutions, such as valproic corrosive, pose a higher hazard. Besides, ladies over 35 a long time ago people who have had a past child with Spina Bifida are more likely to be influenced. Whereas these variables can increment the probability of Spina Bifida, numerous cases happen without a known cause, emphasizing the significance of a solid count of calories, normal pre-birth care, and hereditary counseling to minimize hazards and guarantee ideal results.
Symptoms and Diagnosis
Spina Bifida Symptoms
The indications of Spina Bifida change depending on the sort and seriousness of the condition. In Spina Bifida Occulta, a little tuft of hair or pigmentation may be obvious at the location of the spinal crevice, in more serious cases, such as Meningocele and Myelomeningocele, a sac projects through the infant’s back, with or without a lean layer of skin covering it. The spinal rope tissue may be uncovered in Myelomeningocele.
Associated side effects can include:
- Powerless or paralyzed leg muscles, which may be incapable of moving
- Orthopedic issues like clubfoot, uneven hips, or scoliosis (bent spine)
- Hydrocephalus, characterized by an extended head, bulging delicate spot, and potential brain work impairment
- Seizures
- Bowel and bladder control problems
- Breathing, gulping, or upper arm development difficulties
- Weight administration issues
Diagnosis of Spina Bifida
Prenatal Screening
- Maternal serum alpha-fetoprotein (MSAFP) screening: Measures AFP levels in the mother’s blood to identify potential spinal abnormalities.
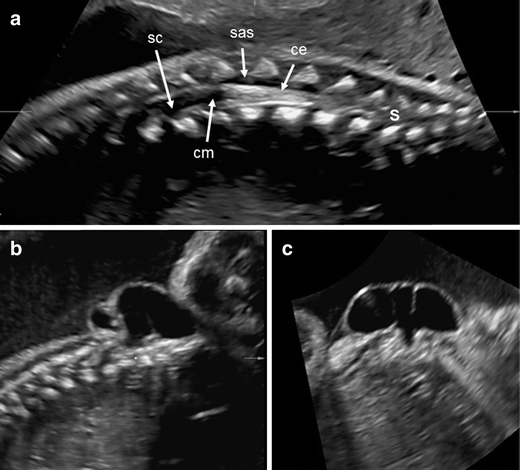
- Ultrasound: Detailed imaging of the fetus to detect spinal defects.
- Amniocentesis: Analyzes amniotic fluid for AFP and other markers to confirm the diagnosis.
Physical Examination at Birth
- Visual inspection for visible signs of Spina Bifida, such as:
- Tuft of hair or birthmark at the base of the spine
- Sac protruding from the back
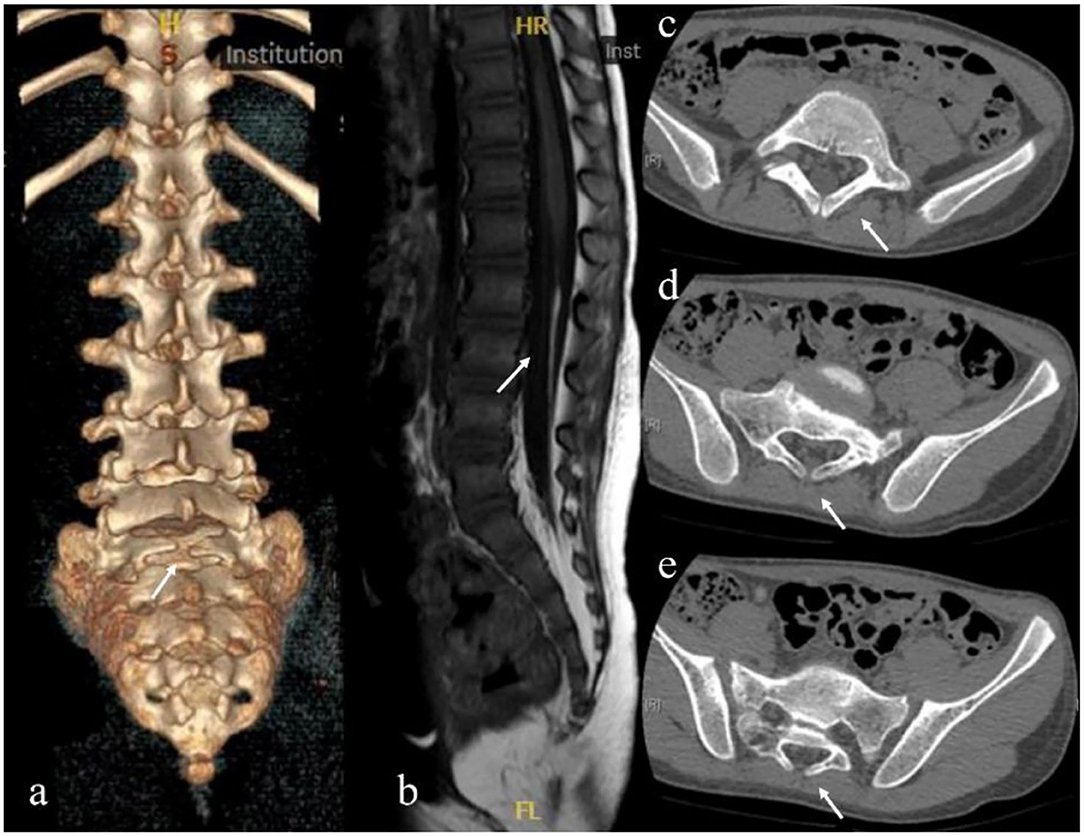
Imaging Tests
- X-rays: Confirms bone abnormalities and spinal defects.
- CT or MRI scans: Evaluates spinal cord damage, hydrocephalus, and other associated conditions.
- Ultrasound: Assesses hydrocephalus and spinal cord abnormalities.
Neurological Evaluation
- Assesses muscle strength, reflexes, and sensation to determine the extent of spinal cord damage.
Reference: Prenatal Diagnosis
Treatment and Management
Treatment and administration of Spina Bifida include a comprehensive approach that addresses the physical, passionate, and social viewpoints of the condition. Surgery plays a significant part in closing the spinal opening, anticipating disease, and repairing related conditions like hydrocephalus. After surgery, recovery treatments take the center to arrange. Physical treatment makes a difference people construct quality, versatility, and adjust, whereas word-related treatment prepares them with abilities for day-by-day living. Discourse treatment addresses communication and gulping troubles, engaging people to express themselves effectively.
Assistive gadgets like wheelchairs, braces, and orthotics upgrade portability, steadiness, and arrangement, permitting people to explore their environment with certainty. Progressing administration is imperative, with standard observing of related conditions and preventative measures like workouts and an adjusted count of calories to keep up with general well-being. Mental back and counseling too play a basic part in tending to enthusiastic and social challenges. A multidisciplinary group of healthcare experts, specialists, and family individuals collaborate to give comprehensive care, and fitting administrations to meet the special needs of each person with Spina Bifida. By taking a dynamic and proactive approach, people with Spina Bifida can lead satisfying lives and reach their full potential.
Complications
Individuals with Spina Bifida face a range of physical, cognitive, and emotional challenges that require proactive management. Hydrocephalus, bladder and bowel control issues, and orthopedic problems like scoliosis and clubfoot can occur, while skin problems and respiratory difficulties like sleep apnea and asthma may also develop. Additionally, learning disabilities, cognitive impairment, ADHD, anxiety, and depression can impact daily life, emphasizing the need for comprehensive support. Related conditions like Chiari II malformation, tethered cord syndrome, syringomyelia, and gastrointestinal and renal issues can also arise, making regular monitoring and multidisciplinary care essential to mitigate these complications and ensure optimal outcomes.
neural tube defects present a complex and multifaceted challenge that requires comprehensive management and care. While these defects pose various obstacles, proactive interventions and multidisciplinary support can significantly enhance the quality of life for affected individuals. Early diagnosis, surgical interventions, rehabilitation therapies, and assistive devices can help alleviate physical complications. Moreover, addressing cognitive, emotional, and psychological aspects through tailored support and resources is vital. By acknowledging the intricacies of neural tube defects and adopting a holistic approach, individuals with these conditions can lead fulfilling lives, reach their full potential, and thrive in their unique journey.