Paralysis is a life-altering condition that influences millions of individuals universally, causing a misfortune of muscle work or versatility. Its onset can be sudden, coming about from a traumatic harm or stroke, or progressive, creating over time due to neurodegenerative infections such as numerous sclerosis or ALS. The effect of loss of motion can change incredibly, influencing any portion of the body, from a single appendage to the whole lower half, and essentially modifying an individual’s daily life. Despite its predominance, loss of motion remains a complex and regularly misjudged condition, with changing degrees of seriousness and effect. This article points to give a comprehensive outline of loss of motion, investigating its sorts, causes, indications, and treatment choices, as well as the most recent inquiries about and progressions in the field, to raise mindfulness and understanding of this multifaceted condition.
Reference: Paralysis
Types of Paralysis
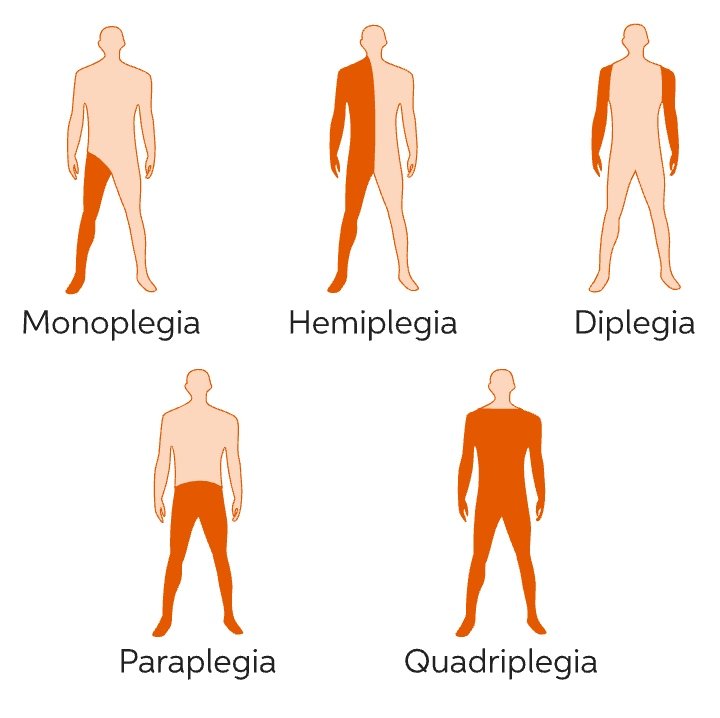
Paralysis can show in different ways, depending on the influenced zone and the degree of the condition. The fundamental categories of loss of motion include:
- Monoplegia: This influences a single appendage, either an arm or leg, and can result from wounds, strokes, or neurological disorders.
- Hemiplegia: This frame includes loss of motion on one side of the body, enveloping both the arm and leg. Hemiplegia frequently stems from brain harm caused by strokes, traumatic brain wounds, or other conditions.
- Diplegia: This sort influences two appendages or sides of the body, commonly both legs or both arms. Diplegia can emerge from spinal rope wounds, different sclerosis, or cerebral palsy.
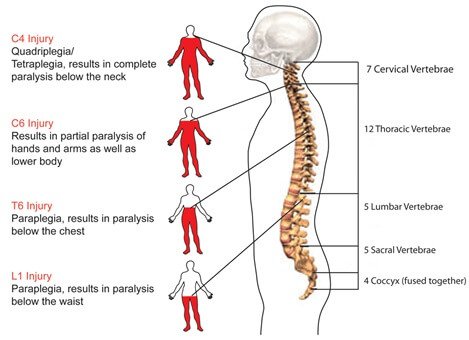
- Quadriplegia: Moreover known as tetraplegia, this extreme shape includes loss of motion of all four appendages. Quadriplegia regularly comes about from disastrous spinal line wounds or progressed neurological disorders.
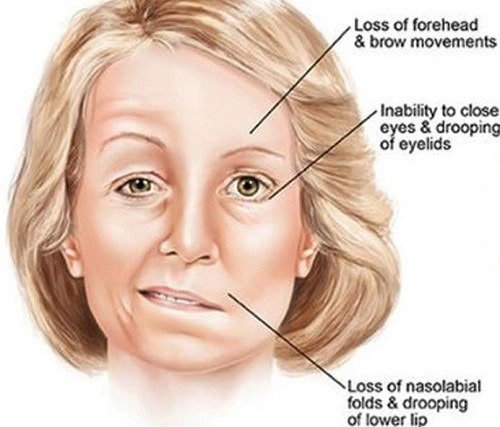
- Facial Loss of motion: This condition influences the facial muscles, driving to shortcoming or loss of motion of facial expressions. Facial loss of motion can be caused by nerve harm, viral diseases, or stroke.
Reference: Types of Paralysis & Facial Paralysis
Causes of Paralysis
Paralysis can arise from a range of underlying factors, including:
- Catastrophic Head Trauma: Severe blows to the head can disrupt the delicate communication between the brain and muscles, potentially leading to paralysis.
- Spinal Cord Damage: Injuries to the spinal cord can sever the vital pathways that transmit nerve signals, resulting in paralysis below the level of injury.
- Cerebrovascular Accidents: Blockages or ruptures in the brain’s blood vessels can cause tissue damage, leading to paralysis.
- Progressive Neurological Disorders: Conditions like ALS and MS gradually erode the nervous system, potentially culminating in paralysis.
- Central Nervous System Infections: Inflammatory responses to infections like meningitis and encephalitis can damage brain tissue and lead to paralysis.
- Space-Occupying Lesions: Abnormal growths, such as tumors and cysts, can compress or destroy surrounding brain or spinal cord tissue, resulting in paralysis.
Symptoms
Paralysis can show through a run of side effects, counting muscle shortcomings, deadness, or shivering sensations in the influenced zone. People may involvement a misfortune of engine control, driving to troubles with development, pose, or coordination. Extra indications may incorporate muscle firmness or fits, reduced reflexes, and weakness or depletion. A few individuals may moreover involve torment or distress in the influenced zone, tangible changes like deadness or shivering, or troubles with discourse or gulping in cases of facial or vocal rope loss of motion. In extreme cases, loss of motion can lead to auxiliary complications, such as respiratory trouble, weight ulcers, or blood clots. If side effects hold on or compound, it is pivotal to look for restorative consideration for appropriate assessment and treatment.
Diagnosis
To diagnose paralysis, healthcare professionals conduct a multifaceted evaluation, incorporating symptom assessment, medical history review, and physical examinations. Advanced diagnostic tools are utilized to confirm the presence and scope of paralysis, including:
- High-resolution imaging technologies like MRI and CT scans to visualize brain and spinal cord anatomy
- Electromyographic testing to measure muscle activity and nerve function
- Nerve conduction velocity studies to assess nerve integrity and function
- Laboratory blood tests to exclude underlying conditions or infections
- Comprehensive physical and neurological examinations to evaluate muscle strength, reflexes, and coordination
Treatment
Effective management of paralysis involves a holistic approach that combines multiple treatment modalities. This may include:
- Targeted medication regimens, featuring muscle relaxants and pain management therapies, to minimize discomfort and maximize comfort
- Personalized physical therapy and rehabilitation protocols, tailored to enhance muscular strength, function, and mobility
- Strategic integration of assistive technologies and adaptive devices, such as wheelchairs, orthotics, and prosthetic solutions, to promote autonomy and facilitate daily activities
- Surgical interventions, like nerve decompression or tendon transfer procedures, aimed at addressing underlying conditions or optimizing muscle function


Reference: Paralysis Treatment & Physical Therapy
paralysis is an intricate and multifaceted condition impacting a significant global population. Its origins can be traced to diverse factors, including traumatic injuries, neurological disorders, and infections. The symptomatology of paralysis encompasses a range of manifestations, from mild muscle weakness and numbness to profound losses of motor control and coordination. A comprehensive diagnostic approach, integrating physical examinations, advanced imaging technologies, and laboratory assessments, is crucial for accurate diagnosis. Effective management and treatment strategies involve a tailored blend of pharmacological interventions, physical therapy, assistive technologies, and surgical procedures. A personalized, multidisciplinary care model can substantially enhance the quality of life for individuals affected by paralysis. By gaining a deeper understanding of the underlying causes, symptoms, diagnostic processes, and treatment options, we can strive to improve the well-being, autonomy, and resilience of those living with paralysis.