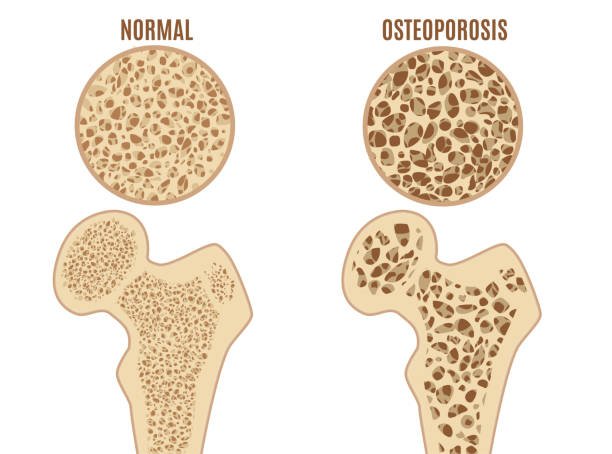
Osteoporosis is a debilitating condition that silently erodes bone density, leaving millions of people worldwide vulnerable to debilitating fractures. Characterized by a gradual thinning of bone tissue, osteoporosis transforms once-strong skeletons into fragile frameworks, prone to shattering under the slightest stress. This insidious disease disproportionately affects older adults, postmenopausal women, and individuals with a history of fractures or family predisposition. As the global population ages, osteoporosis is poised to become an even more pressing public health concern, necessitating urgent attention and proactive measures to prevent, diagnose, and treat this crippling condition.

Reference: Normal and Osteoporotic Bone
Osteoporosis Causes
- Inherited traits: Family history and genetic predisposition play a role in osteoporosis development.
- Hormonal shifts: Declining estrogen levels in women and testosterone levels in men contribute to bone loss.
- Aging process: Bone density naturally decreases with age, increasing osteoporosis risk.
- Lifestyle choices:
- Physical inactivity
- Poor diet (inadequate calcium and vitamin D)
- Smoking habits
- Excessive alcohol consumption
- Underlying medical conditions:
- Rheumatoid arthritis
- Thyroid disorders
- Diabetes
- Kidney and liver disease
- Medication side effects:
- Long-term steroid use
- Anticonvulsant medications
- Chemotherapy
- Certain acid reflux medications
- Nutrient deficiencies:
- Inadequate calcium intake
- Vitamin D deficiency
- Low magnesium levels
- Vitamin K deficiency
- Other contributing factors:
- Small body frame
- Early menopause
- Prolonged immobility or bed rest
Symptoms
As osteoporosis progresses, a range of symptoms can emerge, often subtly at first. Back pain can strike suddenly and severely, or height loss may occur due to compression fractures in the spine. Weakened bones can lead to a noticeable stoop or curvature, making daily activities more difficult. Other signs may include grip strength that’s no longer what it used to be, brittle nails that break easily, or hair that’s thinning. Some people may experience gum recession, loose teeth, or difficulty walking due to osteoporosis-related issues. Chronic pain or aching in the muscles and joints can also become a persistent problem. In advanced cases, the spine may become visibly curved, a condition known as kyphosis. It’s important to note that some individuals may not experience any noticeable symptoms until a fracture occurs, underscoring the importance of preventative measures and regular health check-ups.

Reference: Symptoms
Diagnosis
To diagnose osteoporosis, healthcare professionals take a comprehensive approach. To begin with, they conduct a careful audit of a patient’s restorative history to distinguish potential chance variables and indications. Next, they perform a physical examination to assess posture, mobility, and muscle strength. Additionally, they utilize bone density tests, such as dual-energy X-ray absorptiometry (DXA), to measure bone mineral density. Furthermore, laboratory tests are run to rule out underlying conditions that may contribute to osteoporosis, like thyroid disorders or vitamin D deficiency. Meanwhile, imaging tests, including X-rays, CT scans, or MRI scans, are used to detect any fractures or bone damage. Consequently, a diagnosis of osteoporosis is confirmed when bone density falls below a certain threshold or when one or more osteoporotic fractures have occurred, and other conditions have been ruled out. Ultimately, early diagnosis and treatment can prevent further bone loss and reduce the risk of fractures.
Prevention and Treatment
Avoiding osteoporosis requires a multi-faceted approach. Keeping up a adjusted count calories wealthy in calcium and vitamin D is fundamental, as is locks in in normal work out, such as weight-bearing exercises like strolling or running, and resistance preparing to reinforce muscles. Moreover, dodging smoking and over the top liquor utilization can offer assistance diminish the hazard of osteoporosis. For people with a family history or other hazard variables, pharmaceutical may be endorsed to avoid bone loss.
Treating osteoporosis ordinarily includes a combination of way of life alterations and medicine. Medicines such as bisphosphonates, teriparatide, and denosumab can offer assistance moderate bone misfortune and diminish break hazard. Besides, hormone substitution treatment may be prescribed for ladies with postmenopausal osteoporosis. Way of life changes, counting dietary adjustments, work out programs, and drop avoidance procedures, are too vital. In a few cases, physical treatment may be fundamental to move forward pose, adjust, and quality. By taking a proactive and comprehensive approach, people can successfully oversee osteoporosis and diminish their hazard of fractures.
Special Population
Osteoporosis affects a range of populations, necessitating tailored approaches to prevention and management.
Osteoporosis in Men:
Men are also susceptible to osteoporosis, particularly as they age. Factors like low testosterone levels, certain medical conditions, and lifestyle choices increase their risk. Early detection and intervention are vital to prevent fractures and maintain overall health.
Osteoporosis in Young Adults:
Although less common, osteoporosis can impact young adults due to genetic predispositions, hormonal imbalances, or chronic illnesses. Prompt action and lifestyle modifications can help mitigate risks and promote robust bone development.
Osteoporosis in Postmenopausal Women:
The onset of menopause triggers hormonal fluctuations, accelerating bone loss and increasing osteoporosis risk. Timely interventions, including lifestyle adjustments, hormone replacement therapy (when recommended), and medication, can help safeguard bone health.
Osteoporosis in Individuals with Disabilities:
People with disabilities face distinct challenges in maintaining bone health due to mobility limitations, underlying conditions, or medication side effects. Personalized care plans, adaptive exercise programs, and assistive devices can help address these challenges and prevent osteoporosis-related complications.

Reference: Drug Therapy for Osteoporosis in Older Adults
Delicate bone infection is an inescapable and weakening condition that influences millions around the world. As we age, our skeletal system’s flexibility melts away, clearing out us defenseless to breaks and reduced quality of life. Be that as it may, by recognizing the chance variables and taking proactive measures, we can brace our bones and anticipate this weakening condition. Through a combination of way of life adjustments, dietary alterations, and restorative mediations, we can protect our skeletal wellbeing and keep up our autonomy. By prioritizing bone wellness, we can break free from the shackles of delicate bones and grasp a future filled with imperativeness and mobility.